Powerpoint presentation
Collision Course: IP Rights and Traditional Knowledge Copyright 2005, Douglas Kalish. All rights reserved. Traditional Knowledge • Local, unique to a given culture or society• Contrasts with the international knowledge system generated by universities, research institutions and private firms• Basis for local-level decision making in agriculture, health care, food preparat
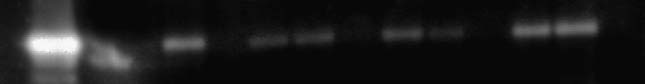 Fig. 2. Changes in endothelial nitric oxide synthase (eNOS) pro-
tein levels. A typical Western blot for eNOS in aortic tissue
with concentrations of eNOS (intensity units/50 mg tissue) in theleft ventricle of rats in heart failure (HF), with and without spiro-
nolactone treatment. First lane, eNOS-positive control; secondlane, HF treated with spironolactone; third and fourth lanes, un-
treated HF; and fifth lane, untreated sham. Note the decrease ineNOS protein levels in untreated HF compared with sham. Spiro-
nolactone treatment restored eNOS level similar to sham control.
Fig. 2. Changes in endothelial nitric oxide synthase (eNOS) pro-
tein levels. A typical Western blot for eNOS in aortic tissue
with concentrations of eNOS (intensity units/50 mg tissue) in theleft ventricle of rats in heart failure (HF), with and without spiro-
nolactone treatment. First lane, eNOS-positive control; secondlane, HF treated with spironolactone; third and fourth lanes, un-
treated HF; and fifth lane, untreated sham. Note the decrease ineNOS protein levels in untreated HF compared with sham. Spiro-
nolactone treatment restored eNOS level similar to sham control.