Draft eln fact sheet v
FACT SHEET PROCTER & GAMBLE USES SAFE DIGITAL SIGNATURE STANDARD FOR ELECTRONIC LABORATORY NOTEBOOK PROJECT To be deployed to up to 4500 P&G scientists and technicians WHAT : Procter & Gamble (P&G) is using the SAFE digital signature standard in its Electronic Laboratory Notebook (ELN) project, reaching potentially 4500 people inside the company. This project is
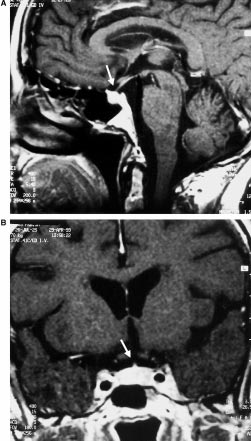 J. Klein et al., Hypophysitis in a 75-year-old woman
Table 1 Pathological blood chemical values at presentation
Corticotropin-Releasing Hormone stimulation. Sim-
ilarly, Thyrotropin-Releasing Hormone stimulation
did not elicit an adequate response of TSH. Finally,
secondary hypogonadism was detected as evidenced
by low FSH and LH baseline levels and the absence
of a significant rise of these hormones after Gona-
dotropin-Releasing Hormone stimulation.
J. Klein et al., Hypophysitis in a 75-year-old woman
Table 1 Pathological blood chemical values at presentation
Corticotropin-Releasing Hormone stimulation. Sim-
ilarly, Thyrotropin-Releasing Hormone stimulation
did not elicit an adequate response of TSH. Finally,
secondary hypogonadism was detected as evidenced
by low FSH and LH baseline levels and the absence
of a significant rise of these hormones after Gona-
dotropin-Releasing Hormone stimulation. Table 2 Results of pituitary function tests at presentation
Plasma hormone levels were measured before (À60, À15), at the time (0), and after (+15, +30, +45, +60, +90) the application of an
intravenous bolus injection of 60 mg CRH, 1.5 mg LHRH, and 12 mg TRH; range of normal values in parenthesis
presentation of 31 years (Beressi et al., 1999; Powrie
et al., 1995). To our knowledge, this is the first report
of a woman 75 years of age presenting with
hypophysitis. Interestingly, we also found elevated
TPO-antibodies in the patient presented. This is in
keeping with previous reports (Barbaro and Loni,
2000; Beressi et al., 1999; Goudie and Pinkerton,
1962; Nagai et al., 1997; Pestell et al., 1990; Sobrinho-
Simoes et al., 1985) and lends support to the
hypothesis of an autoimmune origin of hypophysitis.
Table 2 Results of pituitary function tests at presentation
Plasma hormone levels were measured before (À60, À15), at the time (0), and after (+15, +30, +45, +60, +90) the application of an
intravenous bolus injection of 60 mg CRH, 1.5 mg LHRH, and 12 mg TRH; range of normal values in parenthesis
presentation of 31 years (Beressi et al., 1999; Powrie
et al., 1995). To our knowledge, this is the first report
of a woman 75 years of age presenting with
hypophysitis. Interestingly, we also found elevated
TPO-antibodies in the patient presented. This is in
keeping with previous reports (Barbaro and Loni,
2000; Beressi et al., 1999; Goudie and Pinkerton,
1962; Nagai et al., 1997; Pestell et al., 1990; Sobrinho-
Simoes et al., 1985) and lends support to the
hypothesis of an autoimmune origin of hypophysitis.